클로스트리디움 디피실에 적용하는 약물들
Treatment of Clostridium difficile (C. difficile) infection (CDI) focuses on eradicating the bacteria, controlling the symptoms, and reducing the risk of recurrence. The choice of drugs depends on the severity of the infection and whether it is an initial episode or a recurrent one. Here are the key drugs used to treat C. difficile infections:
1. Vancomycin
- Mechanism: Vancomycin is a glycopeptide antibiotic that inhibits bacterial cell wall synthesis, targeting C. difficile.
- Use: It is the first-line treatment for moderate to severe C. difficile infections and is especially preferred for severe cases or recurrences.
- Administration: Given orally for C. difficile because oral vancomycin stays in the gut where the infection is located, making it effective at treating the bacteria there. Intravenous vancomycin is not effective for CDI.
- Dose: Standard dosing is 125 mg orally every 6 hours for 10 days.
2. Fidaxomicin
- Mechanism: Fidaxomicin is a macrolide antibiotic that inhibits bacterial RNA polymerase, leading to reduced toxin production and C. difficile spore formation.
- Use: It is an effective alternative to vancomycin for both initial and recurrent CDI. It is particularly useful because it is associated with lower rates of recurrence compared to vancomycin.
- Administration: Given orally.
- Dose: Typically 200 mg orally every 12 hours for 10 days.
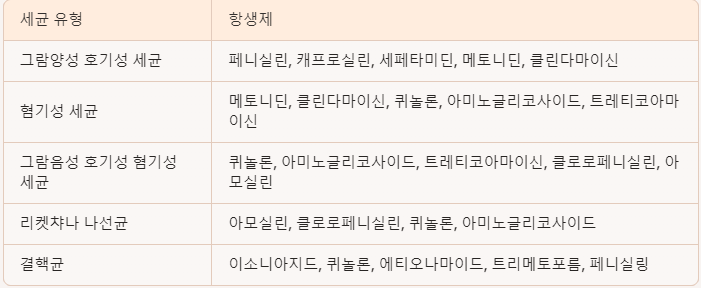
혐기성 세균에 적용할 수 있는 약물
Several antibiotics are effective against anaerobic bacteria, which thrive in low-oxygen environments. Here are some of the most commonly used drugs for treating infections caused by anaerobic bacteria:
1. Metronidazole
- Mechanism: Metronidazole is a nitroimidazole antibiotic that works by generating free radicals that disrupt DNA synthesis in anaerobic bacteria.
- Spectrum: It is highly effective against Gram-negative anaerobes like Bacteroides fragilis and Gram-positive anaerobes like Clostridium species.
- Common Uses: It is often used for intra-abdominal infections, pelvic infections, bacterial vaginosis, Clostridium difficile infection, dental infections, and brain abscesses.
- Administration: Can be given orally or intravenously.
2. Clindamycin
- Mechanism: Clindamycin is a lincosamide antibiotic that inhibits protein synthesis by binding to the 50S ribosomal subunit of bacteria.
- Spectrum: It is effective against Gram-positive anaerobes like Clostridium perfringens and some Gram-negative anaerobes like Bacteroides.
- Common Uses: Clindamycin is used for skin and soft tissue infections, respiratory infections, dental infections, and infections caused by anaerobes in the lungs or abdominal cavity.
- Administration: Available in oral and IV formulations.
3. Carbapenems (e.g., Imipenem, Meropenem)
- Mechanism: Carbapenems inhibit cell wall synthesis and have a broad spectrum of activity.
- Spectrum: They are effective against both Gram-positive and Gram-negative anaerobes, as well as many aerobic bacteria.
- Common Uses: Carbapenems are used for severe mixed infections, including intra-abdominal infections, complicated skin infections, and hospital-acquired infections.
- Administration: Administered intravenously.
4. Beta-Lactam/Beta-Lactamase Inhibitor Combinations (e.g., Piperacillin-Tazobactam, Amoxicillin-Clavulanate)
- Mechanism: These combinations inhibit bacterial cell wall synthesis, with the beta-lactamase inhibitor component protecting the beta-lactam from degradation.
- Spectrum: Effective against Gram-negative anaerobes like Bacteroides and some Gram-positive anaerobes.
- Common Uses: They are often used for polymicrobial infections such as intra-abdominal infections, diabetic foot infections, and aspiration pneumonia.
- Administration: Piperacillin-tazobactam is typically IV, while amoxicillin-clavulanate is available orally.
5. Moxifloxacin
- Mechanism: Moxifloxacin is a fluoroquinolone that inhibits bacterial DNA gyrase and topoisomerase IV.
- Spectrum: It has some activity against anaerobic bacteria, particularly Gram-positive anaerobes.
- Common Uses: Moxifloxacin can be used for respiratory tract infections, skin infections, and complicated intra-abdominal infections where anaerobes are suspected.
- Administration: Available in oral and IV formulations.
6. Cefoxitin and Cefotetan (Second-generation cephalosporins)
- Mechanism: Cefoxitin and cefotetan inhibit bacterial cell wall synthesis.
- Spectrum: These cephalosporins have activity against anaerobes, including some Bacteroides species.
- Common Uses: They are used in surgical prophylaxis, especially for gastrointestinal surgeries, and for intra-abdominal infections.
- Administration: Both are administered intravenously.
Summary of Commonly Used Drugs for Anaerobic Bacteria
- Highly effective for anaerobes: Metronidazole, Clindamycin.
- Broad-spectrum with anaerobic coverage: Carbapenems, beta-lactam/beta-lactamase inhibitor combinations (e.g., Piperacillin-Tazobactam).
- Additional options: Moxifloxacin (for respiratory anaerobes), Cefoxitin (for surgical prophylaxis).
MRSA= 메티실린 저항성 스타필로코쿠스 아우레우스 감염증
Methicillin-resistant Staphylococcus aureus (MRSA) is a challenging bacterial infection due to its resistance to many common antibiotics, including methicillin and other beta-lactams. Treatment options for MRSA depend on the severity of the infection, whether it is a skin and soft tissue infection (SSTI), bloodstream infection, or pneumonia. Here are the key drugs used to treat MRSA infections:
1. Vancomycin
- Mechanism: A glycopeptide antibiotic that inhibits cell wall synthesis by binding to the bacterial cell wall precursors.
- Use: It is the first-line treatment for serious MRSA infections, such as bloodstream infections, pneumonia, endocarditis, and osteomyelitis.
- Administration: Given intravenously for systemic infections; oral vancomycin is used specifically for Clostridium difficile colitis and is not effective for systemic MRSA.
- Monitoring: Requires monitoring of trough levels to ensure therapeutic dosing and avoid nephrotoxicity.
2. Daptomycin
- Mechanism: A cyclic lipopeptide that causes depolarization of the bacterial membrane, leading to cell death.
- Use: Effective for complicated skin and soft tissue infections, bacteremia, and right-sided endocarditis due to MRSA.
- Administration: Given intravenously.
- Note: It should not be used for pneumonia as it is inactivated by lung surfactants.
3. Linezolid
- Mechanism: An oxazolidinone that inhibits protein synthesis by binding to the bacterial 50S ribosomal subunit.
- Use: It is useful for MRSA pneumonia, skin and soft tissue infections, and multi-drug resistant infections.
- Administration: Available in both oral and intravenous forms, making it a versatile option for transitioning from IV to oral therapy.
- Adverse Effects: Long-term use can cause bone marrow suppression, thrombocytopenia, and peripheral neuropathy.
4. Clindamycin
- Mechanism: A lincosamide that inhibits protein synthesis by binding to the 50S ribosomal subunit.
- Use: Effective for mild to moderate MRSA skin infections, abscesses, and as an option for community-acquired MRSA (CA-MRSA). It is particularly useful when an anti-toxin effect is needed, such as in necrotizing infections.
- Administration: Available in both oral and intravenous forms.
- Resistance Testing: It is important to test for inducible resistance (D-test) before using clindamycin for MRSA.
5. Trimethoprim-Sulfamethoxazole (TMP-SMX)
- Mechanism: Inhibits folate synthesis in bacteria, which is crucial for DNA and protein production.
- Use: Often used for mild to moderate MRSA skin and soft tissue infections, including abscesses.
- Administration: Available orally.
- Note: It is not ideal for severe or invasive infections like bacteremia or endocarditis due to its bacteriostatic nature rather than bactericidal.
'약리학' 카테고리의 다른 글
| 항마이코박테리움제, 결핵, 한센병 치료 (1) | 2024.10.23 |
|---|---|
| 항생제 이름을 외워보아요 (0) | 2024.10.22 |
| 핵산합성억제 항생제, 퀴놀론 계열, 비뇨기계통 항생제 (0) | 2024.10.22 |
| 단백질 합성 억제제 항생제 (Protein Synthesis Inhibitors) (3) | 2024.10.21 |
| 페니실린 계열 항생제에 대해 알아봅시다, 세포벽 합성 저해제 (1) | 2024.10.21 |